At-Home Neuromuscular Stimulation to Support Pelvic-Perineal Rehabilitation
Patients seek pelvic-perineal rehabilitation for a variety of reasons. Commonly, these include discomfort due to pelvic organ prolapse (POP), stress urinary incontinence or urgency incontinence, lower back or sacroiliac pain, or simply to regain control of the pelvic floor and ensure a gradual return to sports activities postpartum.
Electrotherapy can be a valuable ally in pelvic-perineal rehabilitation in several ways:
- The use of at-home neuromuscular stimulation for pelvic floor rehabilitation aims to motivate, complement, and maximize home exercises.
- Employing neuromuscular stimulation for pelvic floor rehabilitation aims to prevent compensation by the gluteal or abdominal muscles and to foster motor neuroplasticity.
- Using transcutaneous stimulation of the posterior tibial nerve to address urgency incontinence and detrusor overactivity.
To provide tailored programming and instruction based on the patient's needs, the SET professional team requires close collaboration with the pelvic-perineal physiotherapist.
Thus, by working as a team, the patient will receive recommendations tailored to her needs and best practices for self-administration at home.
NMES AT HOME TO SUPPORT PELVIC-PERINEAL FLOOR REHABILITATION
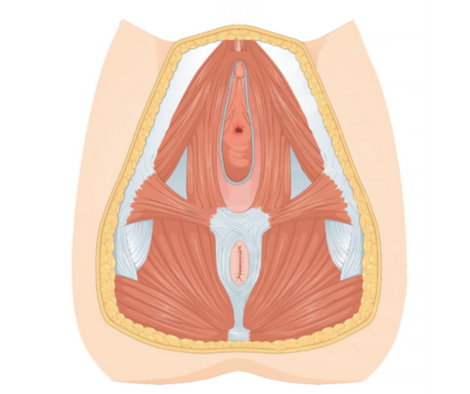
Various factors can lead a patient to seek pelvic-perineal rehabilitation. Among the most common are discomfort associated with pelvic organ prolapse (POP), stress urinary incontinence, lower back or sacroiliac pain, or to regain control over the pelvic floor and ensure a gradual return to sports activities postpartum. These various conditions or symptoms share common factors: a weakness in the pelvic floor's strength, power, endurance, or hypertonia.
Many women struggle to contract their pelvic floor and tend to push instead of drawing in. They might also compensate using their gluteal or abdominal muscles, mistakenly believing they're executing the contraction correctly. Given that the majority of the treatment involves strength and/or relaxation exercises for the pelvic floor at home, it's crucial to ensure the quality of the contraction and the patient's commitment.
The use of NMES for self-care at home can be a facilitator for performing exercises. It can serve as a proprioceptive tool, helping to better understand and optimize the pelvic floor muscle contraction. Indeed, it can be tailored according to the exercises prescribed by the physiotherapist: positioning, parameters in strength, power, or endurance, and use during functional activities or at rest. It can also facilitate the progression of contraction during more challenging movements. Thus, it is personalized according to the patient's needs and can evolve.
To provide tailored programming and instruction based on the patient's needs, the SET professional team requires close collaboration with the pelvic-perineal physiotherapist. Indeed, an assessment of muscle quality, the types of fibers to work on, fatigability, and the ability to relax the muscles is necessary to validate the correct parameters and the number of repetitions to perform with NMES.
By working as a team, the patient will receive recommendations tailored to her needs and best practices for NMES self-administration at home.
USING TENS TO MANAGE OVERACTIVE BLADDER SYMPTOMS?
Urgency urinary incontinence is defined as the involuntary leakage of urine accompanied or preceded by an immediate urge to urinate.
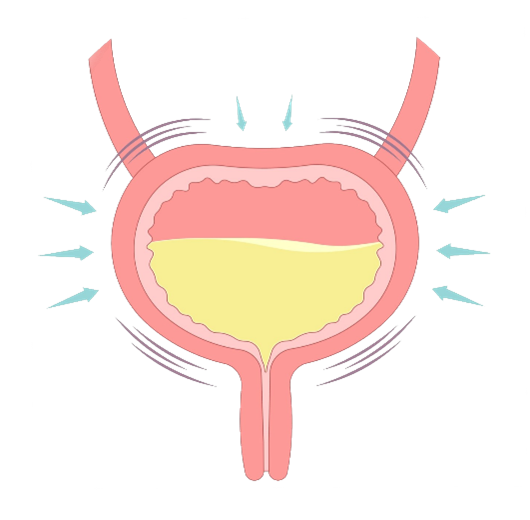
Two mechanisms could be responsible:
- Idiopathic detrusor overactivity, meaning incontinence triggered by spontaneous or induced, yet involuntary, muscle contractions during bladder filling without a defined cause.
- Neurogenic detrusor overactivity, meaning spontaneous or induced, but involuntary, detrusor contractions during bladder filling in the presence of relevant neurological conditions.
It can also be a symptom associated with interstitial cystitis, a chronic pain syndrome predominantly affecting women.
POSTERIOR TIBIAL NERVE TRANSCUTANEOUS STIMULATION (PTNS)
Posterior tibial nerve transcutaneous stimulation is an increasingly researched and utilized option for this population, as the treatment is non-invasive and can be self-administered at home. The method involves placing transcutaneous electrodes near the ankle to stimulate the posterior tibial nerve, which is a branch of the sacral nerve that innervates the bladder and sphincters.
Given that PTNS is minimally invasive, lacks the adverse effects associated with percutaneous stimulation using needles or neuromodulation, and can be self-administered at home, this technique can be a valuable tool for alleviating overactive bladder symptoms.
SET bases its TENS usage procedures on evidence, clinician expertise, and patient feedback.
The protocol involves stimulating the posterior tibial nerve over 12 weeks, three times a week. Since PTNS has not shown to be curative, a maintenance protocol can be continued once a month.
SET provides patient education to facilitate the device's use, self-administration at home, education on the mechanism of posterior tibial nerve stimulation, and adherence to treatment.
SET remains available to support the patient through follow-ups and support services.
At SET, our priority is to assist you in the pelvic-perineal rehabilitation of your patients, focusing on close collaboration to maximize the effectiveness of home treatment. We recognize the importance of clear and precise communication to identify and meet each patient's specific needs.
Thanks to our recommendation tool, we facilitate creating a care plan tailored to your therapeutic goals, thereby enhancing rehabilitation outcomes for the benefit of the patient.
To discover how our expertise in functional electrotherapy can enhance your practice and improve your patients' rehabilitation journey, we invite you to contact one of our experts.
Together, let's advance towards a comprehensive approach from clinic to home for optimal patient outcomes.
Sources:
1. Chronic Pelvic Pain in Women. Dynamed. Accessed March 8, 2022. https://www.dynamed.com/condition/chronic-pelvic-pain-in-women
2. Han X, Shen H, Chen J, Wu Y. Correction to: Efficacy and safety of electrical stimulation for stress urinary incontinence in women: a systematic review and meta-analysis. Int Urogynecology J. 2022;33(5):1363-1363. doi:10.1007/s00192-022-05142-4
3. Barber MD. Pelvic organ prolapse. BMJ. Published online July 20, 2016:i3853. doi:10.1136/bmj.i3853
4. Li Y peng, Cui X, Liu S chen, Zhang S hua, Zhao Y hang. Neuromuscular electrical stimulation for treating postpartum low back pain. Medicine (Baltimore). 2018;97(28):e11426. doi:10.1097/MD.0000000000011426
5. Rééducation périnéale et pelvienne: 5 fausses croyances. OPPQ. Accessed March 7, 2023. https://oppq.qc.ca/blogue/reeducation-perineale-et-pelvienne-fausses-croyances/
6. Allon EF. The role of neuromuscular electrical stimulation in the rehabilitation of the pelvic floor muscles. Br J Nurs. 2019;28(15):968-974. doi:10.12968/bjon.2019.28.15.968
7. Corcos J, Przydacz M, Campeau L, et al. CUA guideline on adult overactive bladder. Can Urol Assoc J. 2017;11(5):142. doi:10.5489/cuaj.4586
8. Ghavidel-Sardsahra A, Ghojazadeh M, Rahnama’I MS, et al. Efficacy of percutaneous and transcutaneous posterior tibial nerve stimulation on idiopathic overactive bladder and interstitial cystitis/painful bladder syndrome: A systematic review and meta-analysis. Neurourol Urodyn. 2022;41(2):539-551. doi:10.1002/nau.24864
9. Zhao J, Bai J, Zhou Y, Qi G, Du L. Posterior Tibial Nerve Stimulation Twice a Week in Patients with Interstitial Cystitis. Urology. 2008;71(6):1080-1084. doi:10.1016/j.urology.2008.01.018
10. Yang DY, Zhao LN, Qiu MX. Treatment for overactive bladder: A meta-analysis of transcutaneous tibial nerve stimulation versus percutaneous tibial nerve stimulation. Medicine (Baltimore). 2021;100(20):e25941. doi:10.1097/MD.0000000000025941
Connectez avec nous sur les médias sociaux